Successfully removing dressings can be beneficial for wound care.
It is one thing to apply wound care products that are necessary to heal an injury, but it’s equally important to properly remove applied products when changing the dressing.
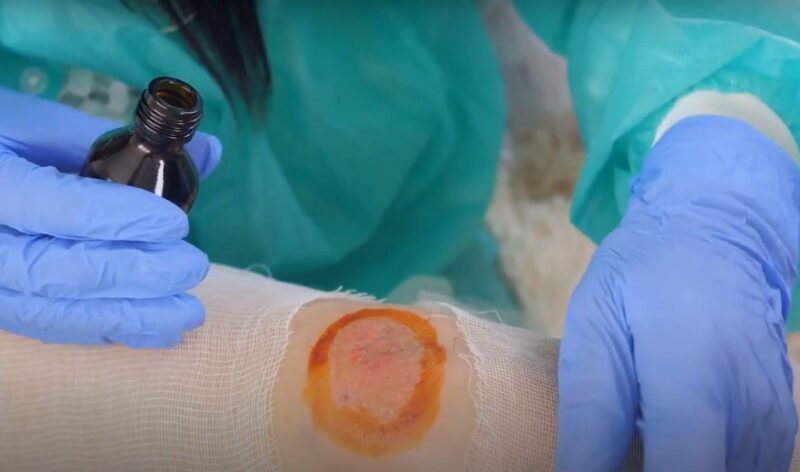
Part of this process may include efficiently cleaning the damaged tissue to avoid a wound infection and appropriately unraveling a covering or layer of gauze, all of which are crucial in treatment. Here are a few guidelines to consider when removing your wound care products.
Minimization

When changing your wound care dressings, it is best to keep dressing changes at a minimum and of course follow your clinicians change instructions. Many advanced wound care dressings are typically slated to last multiply days, and there is no need to over pack your wound with dressing, which will only further complicate the removal process.
Your dressing may become dried up, so if this is the case remembering to soak the bandage in saline or a salt water solution will loosen the covering.
Reducing Pain Through Self-Guided Therapy
For more severe wounds, such as diabetic pressure ulcers or lesions in a chronic stage, dressing removal can be a fairly painful experience.
This is where different forms of at-home therapeutic treatment can be useful. Relaxation techniques are recommended by the National Center for Complementary and Alternative Medicine as an effective way to minimize the amount of pain experienced during bandage removal.
Taking deep slow breaths, focusing on your heartbeat or visualizing guided imagery that evokes pleasant thoughts are encouraged forms of therapy to administer while changing a dressing due to the calming effect they can offer your body during pain sensations.
Monitoring the Wound
- Before removing the dressing, it’s crucial to assess the condition of the wound. Look for signs of healing or any indications of infection like increased redness, swelling, or discharge.
- Take note of any changes in the wound’s appearance since the last dressing change. This information can be vital for healthcare providers in tracking the healing process.
Preparing the Area
Ensure that the area around the wound is clean and free of debris. This minimizes the risk of introducing bacteria into the wound during dressing changes. Use a clean, dry towel or cloth to gently pat the area around the wound, keeping it dry and ready for the new dressing.
Gentle Removal Techniques

If the dressing is adherent, you can use a sterile saline solution or a doctor-recommended wound cleanser to moisten the dressing, making it easier to remove without causing trauma to the wound.
Gently lift the edges of the dressing and peel it back slowly, ensuring not to pull on the skin or the wound itself.
Disposing of the Old Dressing
- Dispose of the used dressing in a sanitary manner. Used dressings can contain harmful bacteria and should be handled with care.
- After removing the dressing, wash your hands again to prevent the spread of any bacteria.
Applying the New Dressing

- When applying a new dressing, handle it by the edges and avoid touching the part that will be in contact with the wound.
- Place the dressing gently over the wound, ensuring it covers the entire area and adheres well to the surrounding skin without causing tension.
Pain Management During Dressing Change
- For those experiencing significant discomfort during dressing changes, over-the-counter pain medication taken prior to the procedure can help ease the pain. Always consult with your healthcare provider before taking any medication.
- Utilize the relaxation techniques mentioned earlier not only during, but also before starting the dressing change to help alleviate anxiety and discomfort.
Post-Dressing Change Care

After applying the new dressing, monitor the wound for any signs of reaction to the dressing material, such as increased redness, itching, or unusual discomfort.
Keep a record of each dressing change, noting the wound’s appearance, any issues encountered during the change, and your pain levels. This log can be a valuable tool for your healthcare provider.
FAQ
How often should a wound be checked for signs of infection?
Wounds should be checked daily for signs of infection, such as increased pain, redness, swelling, or pus. If any of these symptoms are present, consult a healthcare provider immediately.
Can you shower or bathe with a wound dressing?
It depends on the type of dressing. Some are waterproof, but others may need to be kept dry. Always follow the specific instructions provided by your healthcare provider.
What should you do if you’re allergic to a wound dressing material?
If you notice signs of an allergic reaction, such as itching or a rash, remove the dressing and contact your healthcare provider. They can recommend an alternative dressing material.
Is it safe to use home remedies on a wound before dressing it?
Home remedies should be used with caution. Some substances can irritate the wound or delay healing. Always consult a healthcare provider before applying any home remedy.
How can you tell if a wound is healing properly?
Signs of proper healing include a gradual decrease in pain, reduction in wound size, and formation of new, healthy tissue. If the wound does not seem to be healing, consult a healthcare provider.
Can diet impact wound healing?
Yes, a nutritious diet rich in vitamins and proteins can support wound healing. Stay hydrated and consider foods high in Vitamin C, zinc, and protein.
What should you do if a wound starts bleeding during a dressing change?
Apply gentle pressure with a clean cloth or gauze for a few minutes. If the bleeding does not stop or is heavy, seek medical attention immediately.
Final Words
Proper wound care and dressing techniques are essential for healing. Understanding how to manage and care for wounds can significantly improve recovery and prevent complications.







