Depending on the drainage, this component of wound healing can actually be a sign of success.
Though not always the case, a large number of open wounds experience drainage, or as it’s called by physicians, exudate. Though this secretion of fluids is part of a normal wound-healing process, it can also indicate the presence of harmful infections or any unhealthy inflammation.
As such, it’s important to understand the various types of wound drainage to better grasp just what your average wound care regimen might entail. Here are the three most common types of wound exudate:
Sanguineous drainage
Composed primarily of blood, sanguineous drainage is generally bright in color and rather thick in its overall consistency, with some comparisons being made to syrup. This specific drainage is most common in deep partial-thickness and full-thickness wounds. During the inflammation stage of the healing cycle, a little bit of sanguineous drainage is normal as it indicates proper circulation.
However, if you’re still experiencing drainage after a few hours, it can indicate trauma to the wound site. Serosanguineous drainage features added plasma, which makes the run-off appear pink in color. Serosanguineous exudate is usually indicative of damage to blood vessels and capillaries.
Serous drainage

The result of protein and other fluids found in human tissue, serous drainage is generally clear in color, though it can occasionally have a slightly brownish hue. A minimal amount of serous drainage is not only normal, but actually important, as this drainage contains sugars, white cells, proteins and several other chemicals that are vital for the healing process.
However, too much serous exudate can indicate a high level of bioburden, which relates to an abundance of potentially harmful bacteria and other microorganisms.
Purulent discharge
Unlike the aforementioned discharge types, purulent is almost never part of a normal and healthy wound care regimen. That’s because this form of drainage contains components like pus, white blood cells, dead bacteria and various inflammatory cells, all signs of an infection. In fact, as the infection worsens, the purulent discharge will increase in both capacity and overall consistency.
Fortunately, it’s easy to discern purulent’s harmful nature given that it’s either yellow, brown or sickly green in color. By the time the drainage has become seropurulent – which is more translucent in hue but considerably much thicker in consistency – the wound is very likely infected and will require significant intervention.
Measuring drainage
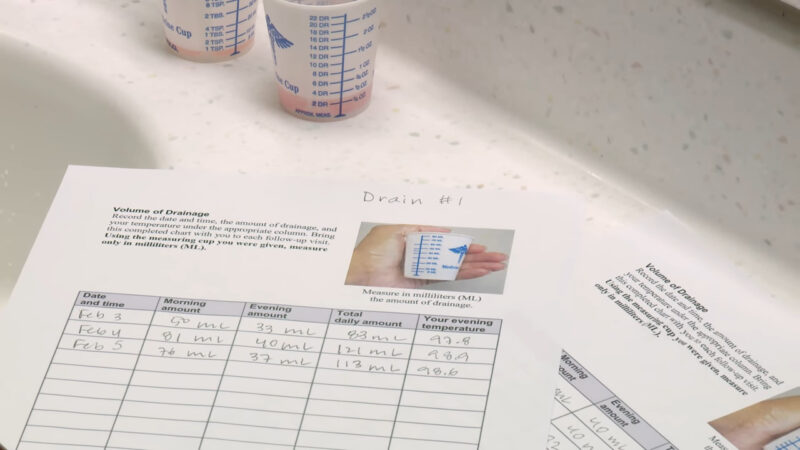
Not only do doctors pay attention to the color and consistency of the wound, but the amount of actual drainage is just as vital in diagnosing issues. As Wound Care Advisor pointed out, levels of drainage are broken down by the percentage of total saturation:
- Scant drainage: Far below 25 percent saturation, which means dressings are only slightly moist.
- Minimal drainage: Usually no more than 25 percent saturation, and dressings are considered mostly damp.
- Moderate drainage: Anything between 25 percent and 75 percent saturation, which means dressings are soaked.
- Copious drainage: The most severe level, which includes 75 percent saturation. Serious intervention is almost always required.
Fibrinous Drainage
Fibrinous drainage is typically seen in wounds that are healing slowly or have become chronic. This type of exudate is characterized by a thick, clotted appearance, somewhat like fibrin, the protein involved in blood clotting. It usually has a yellowish-white color and can be indicative of a wound that is not progressing through the normal stages of healing.
Fibrinous drainage may signal that the wound environment needs to be re-evaluated and possibly that debridement (removal of dead or non-viable tissue) may be necessary to promote healing.
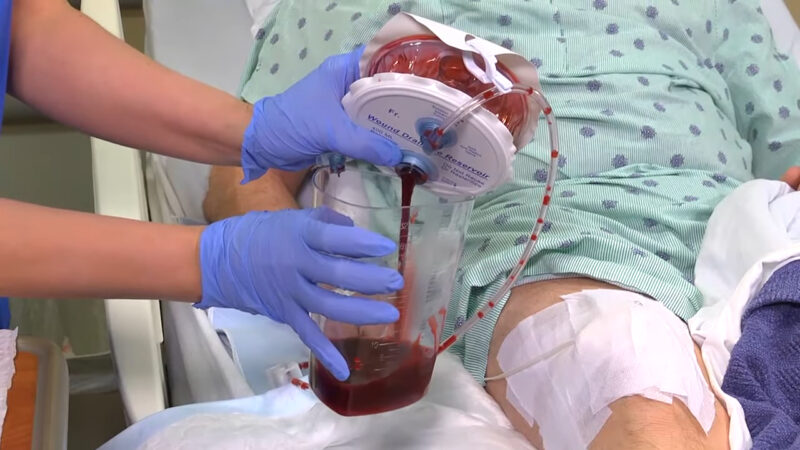
Hemorrhagic Drainage
- Hemorrhagic drainage is predominantly composed of blood, similar to sanguineous drainage, but is typically seen in greater volume.
- This type of drainage often occurs in wounds that have reopened or have been subject to new trauma.
- The color is a vivid red, indicating fresh bleeding, and if the drainage is persistent or voluminous, it may suggest a serious complication such as a ruptured blood vessel or an underlying coagulation disorder.
- Immediate medical attention is often required for wounds exhibiting hemorrhagic drainage to prevent excessive blood loss and to address the underlying cause.
Additionally, doctors pay attention to the odor of the wound site, specifically its strength and any specific smells, like fecal matter or general mustiness.
For wounds with particularly high levels of drainage, you’ll need to rely on the latest in wound dressing technologies. That’s where Advanced Tissue comes in. As the nation’s leader in the delivery of specialized wound care supplies, Advanced Tissue promptly ships supplies to individuals at home and in long-term care facilities.
FAQ
Can diet or nutrition impact wound healing and drainage?
Yes, nutrition plays a crucial role in wound healing. A balanced diet rich in protein, vitamins (especially Vitamin C and A), and minerals like zinc can enhance the body’s ability to repair tissue and manage wound exudate effectively.
How often should wound dressings be changed?
The frequency of dressing changes depends on the wound type, the amount of drainage, and the type of dressing used. Typically, dressings should be changed when they become saturated or as advised by a healthcare professional.
Are there any natural remedies that aid in wound healing?
Some natural remedies, such as honey and aloe vera, have properties that can aid in wound healing. However, it’s essential to consult with a healthcare provider before using any natural remedies, especially for severe wounds.
How does smoking affect wound healing?
Smoking can significantly impede wound healing. It reduces blood flow and oxygen supply to the wound site, delaying healing and increasing the risk of infection.
What are the signs of an infected wound?
Signs of an infected wound include increased redness, warmth, swelling, pain, purulent discharge, foul odor, and sometimes fever. Immediate medical attention is necessary if infection is suspected.
Can stress affect wound healing?
Yes, high levels of stress can negatively impact wound healing. Stress hormones can slow down the healing process by affecting the immune response and inflammation.
Is it safe to exercise with a healing wound?
Moderate exercise can be beneficial for wound healing, as it improves blood circulation. However, it’s essential to avoid putting direct pressure or strain on the wound area and to consult with a healthcare provider for specific recommendations.
Final Words
Understanding different types of wound drainage is crucial in effective wound care. Monitoring exudate type, consistency, and amount is essential for successful healing. Always seek professional medical advice for proper wound management.







