As surgical wounds are healing, there are often some distinct changes that occur to the skin both around and near the wound. While this surgical wound healing is nothing to be embarrassed about – your body is properly caring for itself – there are some warning symptoms to keep watch for.
Here are a few things that you can expect – and the things to watch out for:
1. Fluid
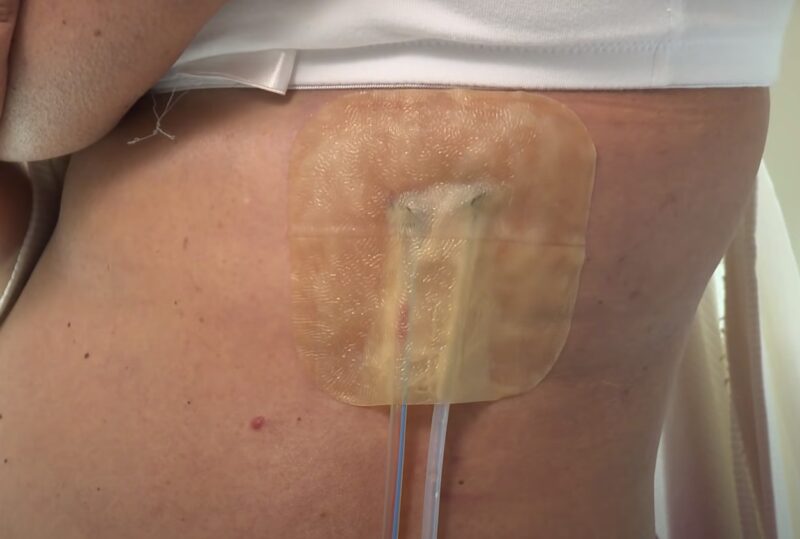
After a surgical procedure, it’s common and healthy for some fluid to drain from the incision site. This drainage is a natural part of the body’s healing process. Typically, you can expect clear or slightly yellow fluid for the first two to three days post-surgery.
This fluid is usually thin and slightly watery, indicating that your body is healing as expected. Another type of drainage you might encounter is serosanguinous drainage. This fluid is slightly pink due to the presence of blood cells. It’s not a cause for alarm. Rather, it’s a normal part of the healing process, especially in the initial stages post-surgery.
When Drainage Indicates a Problem
However, not all types of drainage are positive signs. If you observe green, yellow, or cloudy drainage, it could be an indication of an infection at the surgical site. This type of drainage often differs in consistency and color from the normal, thin, and watery fluid.
Taking Action
If you notice any concerning changes in the drainage from your wound, such as a shift in color or consistency, it’s crucial to contact your healthcare provider or clinician immediately. They can assess the situation and advise on the next steps, which may include changing your wound care routine or prescribing medication to address a potential infection.
Proactive Measures
Always monitor the wound site closely in the days following your surgery. Keeping the area clean and following your doctor’s instructions for wound care are essential steps in preventing infection and ensuring a smooth healing process.
If you’re unsure about what type of drainage is normal or if something you observe seems unusual, don’t hesitate to reach out to your healthcare provider for guidance. Early intervention is key to addressing potential complications and promoting effective healing.
2. Redness

Experiencing a certain degree of redness and inflammation around a surgical wound is a typical response of the body post-procedure. This discoloration is a part of the body’s natural healing process. The tissue around the altered area reacts to the surgery, resulting in redness as blood flow increases to aid in healing and regeneration.
Generally, this redness is localized and should start to diminish within about six months, although the exact timeline can vary depending on the severity and nature of the surgical procedure.
When Redness Is a Concern
However, not all redness is a benign sign. While it’s normal to have some redness directly around the wound site, be vigilant for any redness that starts to spread beyond the immediate area of the wound.
If you notice the redness expanding into splotches or forming thready, spider web-like patterns, this could be indicative of an infection. Such spreading redness, especially if accompanied by increased pain, warmth, swelling, or discharge, requires immediate medical attention.
Taking Action
In cases where the redness is spreading or changing in character, it’s crucial to seek medical advice without delay. Your healthcare provider can assess the wound to determine if an infection is present and advise on the appropriate course of action.
This might include prescribing antibiotics, changing your wound care regimen, or using specific types of wound dressings designed to manage infection.
Proactive Measures
To minimize the risk of infection and ensure proper healing, it’s important to follow all post-surgical care instructions provided by your healthcare team. Keep the wound clean and dry, adhere to any prescribed wound dressing changes, and monitor the area regularly for any signs of change.
If you’re uncertain about what you’re seeing or if something seems unusual, don’t hesitate to contact your healthcare provider for guidance. Early detection and treatment of potential complications are key to a successful recovery.
3. Raised Skin

Scarring is a common and expected outcome following most surgical procedures. It’s a natural part of the body’s healing process. When your body heals a wound, it produces collagen to close and strengthen the incision site. This collagen buildup often results in raised skin directly over the wound.
Additionally, the skin around the scar may feel tighter as it’s pulled together during the healing process. These scars can vary in size and appearance based on the type of surgery, the location of the incision, and individual healing factors.
When Raised Skin Indicates a Problem
However, not all changes in the skin’s texture are normal. If you notice excessive raised skin, especially if it’s accompanied by redness, warmth, or pain, it could be a sign of an underlying issue like an infection or abnormal scarring, such as keloids or hypertrophic scars.
Monitoring Lymph Nodes
Another important aspect to consider is the condition of the lymph nodes near the surgical site. When a wound is infected, the closest lymph nodes may become enlarged as part of the body’s immune response. Regularly checking these lymph nodes can help in early detection of an infection.
If you feel that the lymph nodes are swollen, tender, or enlarged, it’s important to seek medical attention.
Taking Action
If you have concerns about the appearance of your scar, the texture of the skin around your surgical site, or the condition of nearby lymph nodes, it’s advisable to consult with your healthcare provider.
They can assess whether these changes are part of the normal healing process or if they indicate a complication that needs medical intervention.
Proactive Measures
To promote healthy scarring and reduce the risk of complications, follow your surgeon’s post-operative care instructions. This may include using prescribed scar treatment creams, avoiding direct sunlight on the scar, and gentle massage to keep the skin supple.
Remember, each person’s body heals differently, and what is normal for one person may not be for another. Keeping an open line of communication with your healthcare provider throughout your recovery is crucial for addressing any concerns that may arise.
FAQs
What does a bad healing wound look like?
A poorly healing wound may appear excessively red, swollen, or produce abnormal drainage like green or yellow pus. It might also feel warm or painful, and show signs of reopening or not closing properly.
What color should a healing incision look like?
A healthy healing incision typically looks pink or red and gradually fades to a paler color. Initially, it may be slightly swollen and red, but this should improve over time, not worsen.
How long can a surgical incision take to heal?
The healing time for a surgical incision varies depending on the surgery type, location, and individual health factors. Generally, primary healing may take up to three months, while complete internal healing can take up to several months.
What is the hardest wound to heal?
Chronic wounds, like diabetic ulcers or pressure sores, are often considered the hardest to heal due to underlying health conditions, poor circulation, or prolonged pressure, which impede the normal healing process.
Summary
Distinguishing between a healing and an infected surgical wound is crucial for a successful recovery.
The three key indicators to watch for are the nature of drainage, the extent and character of redness, and changes in the skin around the wound, particularly in terms of raised areas or scarring.
Normal healing involves clear or slightly yellow drainage, localized redness, and typical scarring with raised skin.







